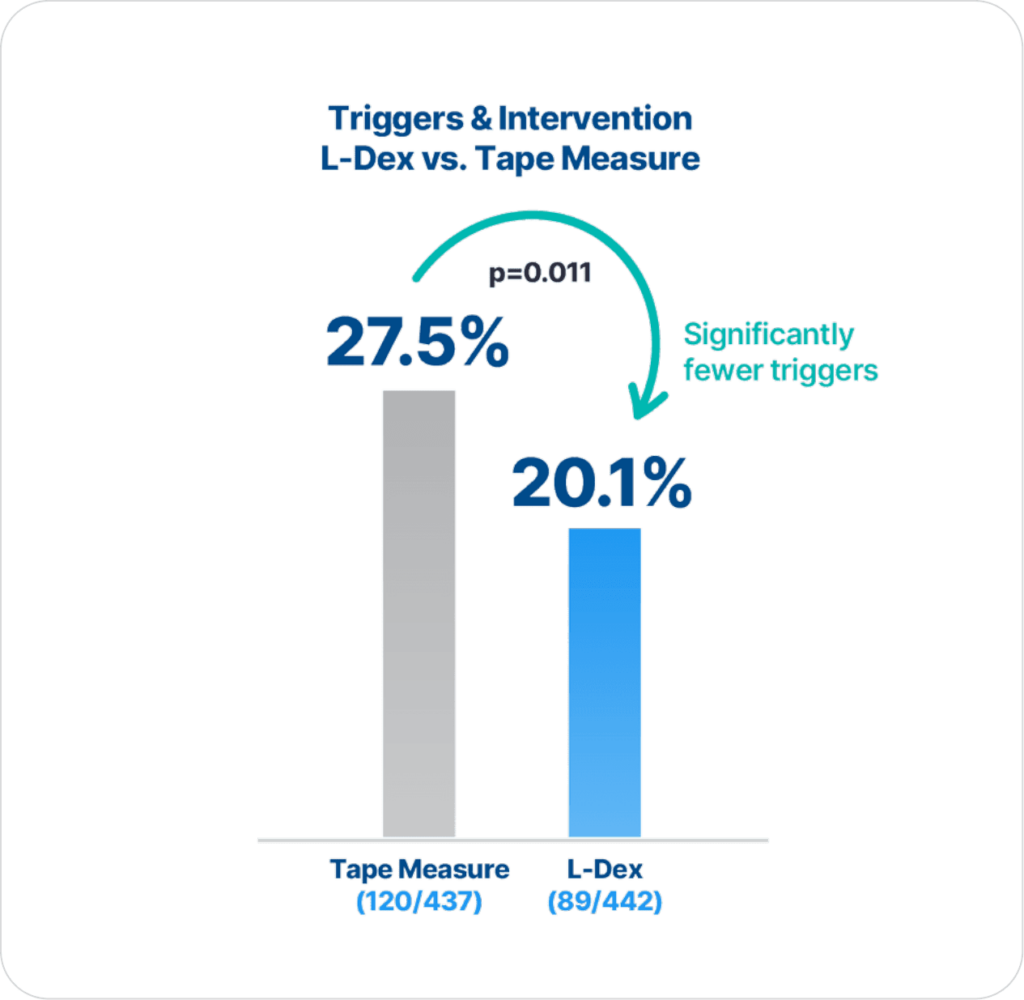
ImpediMed’s BIS technology is more precise and reliable than tape measure in detecting lymphedema (LE), as there are statistically significantly fewer triggers and interventions for those assessed with BIS compared to tape measure (p=0.011)2.
Extensive clinical evidence shows that using ImpediMed’s bioimpedance spectroscopy (BIS) technology for early detection and intervention reduces the impact of chronic lymphedema on breast cancer patients.
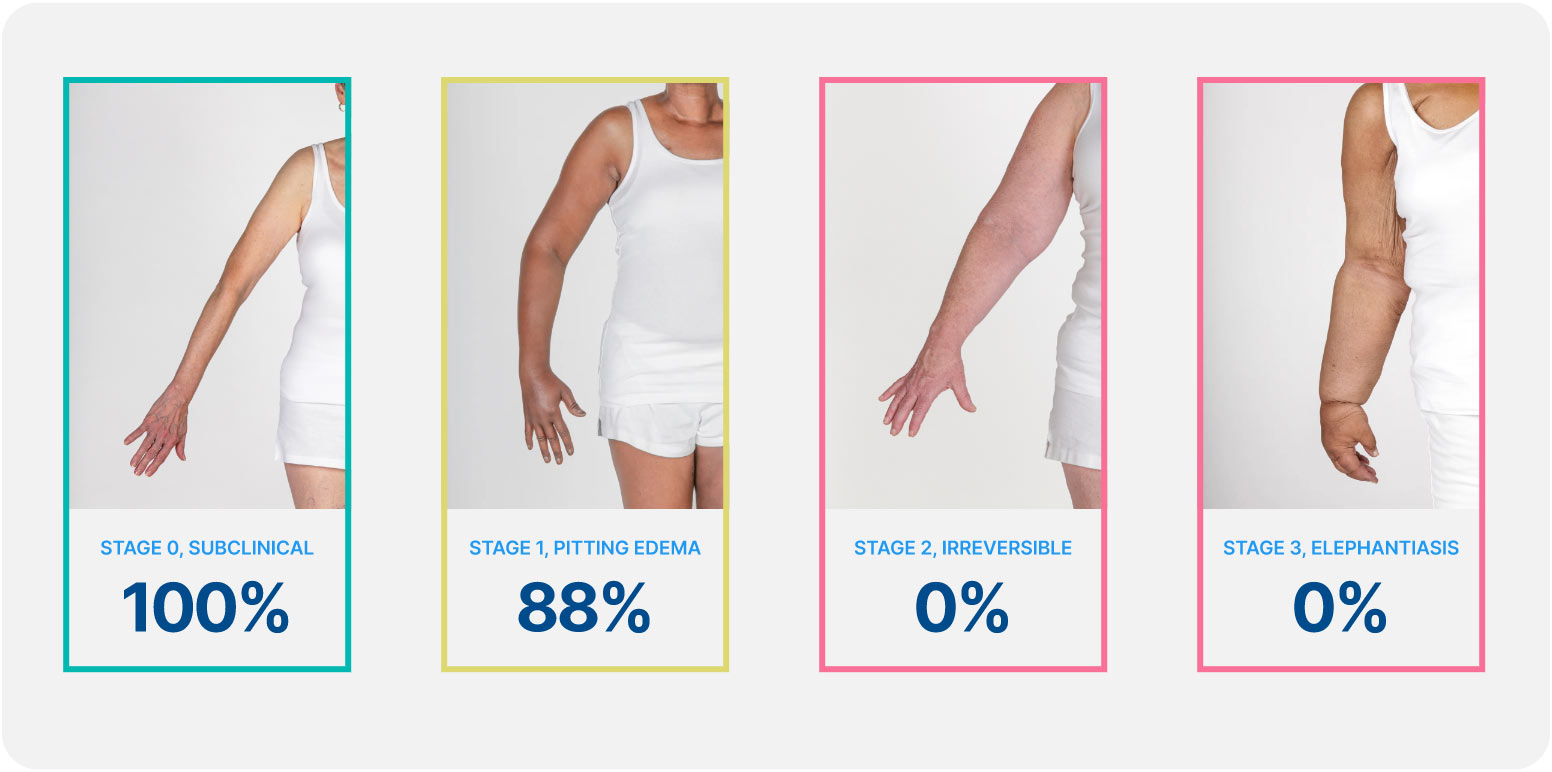
Lymphedema develops in stages, and a university of Kansas study found that when lymphedema is detected at stage 0 or stage 1 it is reversible, but in stages 2 and 3 it is not. These findings demonstrate how early conservative intervention and prospective monitoring with BIS can significantly lower rates of BCRL and persistent BCRL (pBCRL).¹
The PREVENT Trial involved 10 centers across the US and Australia and was the largest randomized controlled trial (RCT) to assess lymphedema prevention in breast cancer patients.
These clinical practice guidelines present clinicians with a standardized evidence-based approach to BCRL surveillance to detect subclinical BCRL, allowing for early intervention and low rates of chronic BCRL.
Open access: YesAmerican Society of Breast Surgeons (ASBrS) Lymphatic Surgery Working Group Agrees: Evidence Supports Programs for Early Detection and Intervention to Prevent Chronic Lymphedema.
Open access: YesThe Kaplan–Meier analysis shows that patients with early detection using L-Dex and intervention have statistically significant higher rates of lymphedema progression free survival through three years compared to using tape measure. This reinforces the importance of monitoring patients for three years, since progression to chronic lymphedema occurred throughout the three-year follow up period.
Open access: YesPatients underwent a compression (sleeve and gauntlet) intervention for subclinical breast cancer-related lymphedema (S-BCRL). Physical, emotional, and quality-of-life (QoL) outcomes were examined. Associations of change in extracellular fluid alone through bioimpedance spectroscopy (BIS) or change in whole-arm volume through tape measure with the outcomes at time of S-BCRL were explored.
Open access: YesThe results confirm known BCRL risk factors such as axillary lymph node dissection, taxane-based chemotherapy, regional nodal irradiation, and obesity and provides novel data on the increased risk of BCRL in patients living in a rural areas as well as no increased risk from air travel.
Open access: YesThis study compared rates of progression to chronic breast cancer-related lymphedema (defined as ≥ 10% arm volume change from baseline requiring complex decongestive physiotherapy [CDP]) following an intervention for subclinical lymphedema (S-BCRL) triggered by bioimpedance spectroscopy (BIS) or by tape measurement (TM).
Open access: YesPart 1: Definitions, Assessments, Education, and Future Directions
Open access: YesThis is the first study to utilize BIS measurements to assess response to LVB surgical intervention for BCRL. BIS measurements demonstrated clinically significant improvement after LVB, providing objective evidence in support of this surgical treatment for BCRL. BIS changes should be reported as key objective data in future studies assessing BCRL interventions, including response to LVB.
Open access: NoThe NCCN Guidelines® are consistent with regard to the necessity to educate patients about lymphedema and monitor for the early development of lymphedema.
Open access: YesThe lower triggering rates with BIS and its better discrimination of the risk of sBCRL by receipt and type of RNI compared with TM support its use for post treatment surveillance to detect sBCRL and to initiate early intervention. The risk of sBCRL increased with more extensive axillary treatment. Patients having ALND or extensive RNI require close surveillance for BCRL. Longer follow-up is required to determine rates of progression to clinical lymphedema.
Open access: YesEvidence suggests that monitoring with BIS allowing for early intervention significantly reduces the relative risk of chronic BCRL with a 69% and 81% reduction compared to background and circumference, respectively. Circumference monitoring did not appear to provide a benefit with respect to chronic BCRL incidence. Based on these results, BIS should be considered for BCRL screening in order to detect subclinical BCRL and reduce rates of chronic BCRL, particularly in high-risk patients.
Open access: YesThe findings support impedance measurements being made reliably using either the lead or stand- on device, representing supine and upright measurement positions, respectively. Data between devices were, however, not directly interchangeable.